In recent years, intermittent fasting has surged in popularity as a strategy for weight management and overall health. But what about its impact on cardiovascular risk? If you’re curious about how this eating pattern affects heart health, you’re in the right place.
Let’s explore the relationship between intermittent fasting and cardiovascular risk, shedding light on both potential benefits and concerns.
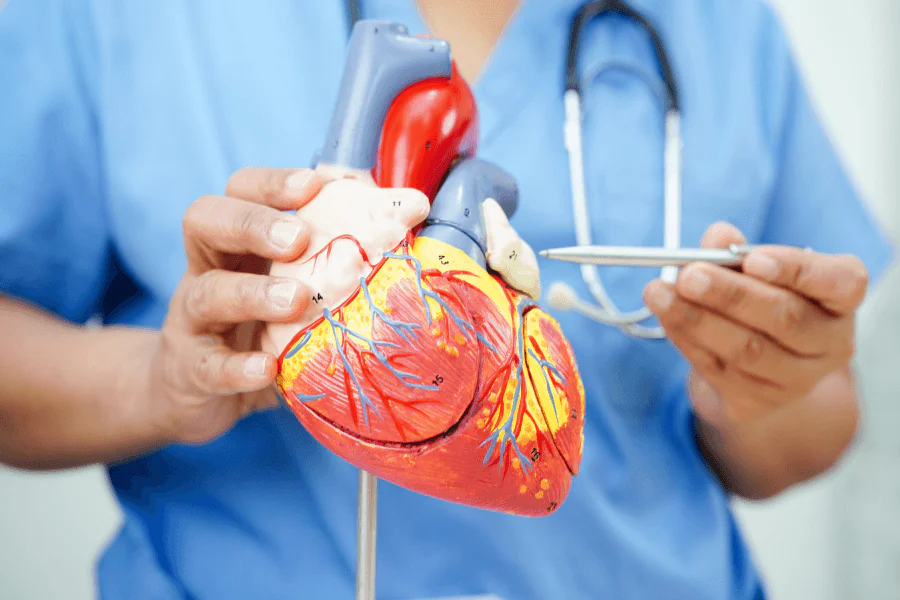
What is Cardiovascular Risk?
Cardiovascular risk refers to the probability of experiencing cardiovascular diseases (CVD), including heart disease, stroke, and hypertension, due to various risk factors. It is a measure used to assess the likelihood of adverse heart-related conditions, such as heart disease, stroke, or high blood pressure. This risk is influenced by a variety of factors, including:
- High blood pressure (Hypertension)
- High cholesterol levels
- Smoking
- Obesity
- Sedentary lifestyle
- Family history of heart disease
- Diabetes
- Unhealthy Diet
- Age
- Gender
- Stress
Measuring Cardiovascular Risk
- Risk Assessment Tool
- Biomarkers
By understanding these risk factors, we can better evaluate how lifestyle changes, like intermittent fasting, might impact heart health.
Strategies for Reducing Cardiovascular Risk
- Healthy Diet
- Regular Exercise
- Smoking Cessation
- Weight Management
- Blood Pressure Control
- Cholesterol Management
- Diabetes Management
- Stress Management
What is Intermittent Fasting?
Intermittent fasting (IF) is an eating pattern that alternates between periods of fasting and eating. Unlike traditional diets, which focus on what you eat, intermittent fasting emphasizes when you eat. It involves cycling between periods of eating and fasting. It doesn’t prescribe specific foods but rather sets time windows for eating and fasting.
How to Incorporate Intermittent Fasting into Your Lifestyle
Types of Intermittent Fasting Protocols
Choosing the right intermittent fasting method can depend on your personal preferences and health goals. Here’s a brief overview of different protocols:
16/8 Method:
- How It Works: Fast for 16 hours and eat during an 8-hour window.
- Example: Skip breakfast and eat between 12 PM and 8 PM.
5:2 Method:
- How It Works: Eat normally for five days of the week and consume only about 500-600 calories on two non-consecutive days.
- Example: Eat normally on Monday, Wednesday, Friday, Saturday, and Sunday; restrict calories on Tuesday and Thursday.
Eat-Stop-Eat:
- How It Works: Fast for 24 hours once or twice a week.
- Example: Fast from dinner one day to dinner the next day, twice a week.
Alternate-Day Fasting:
- How It Works: Alternate between days of regular eating and days of fasting.
- Example: Eat normally on Monday, Wednesday, Friday, and fast on Tuesday, Thursday, Saturday.
Warrior Diet:
- How It Works: Fast for 20 hours and eat during a 4-hour window.
- Example: Eat a small amount of fruits and vegetables during the day and consume one large meal in the evening.
OMAD (One Meal a Day):
- How It Works: Eat only one meal a day and fast for the remaining 23 hours.
- Example: Have a large meal at dinner and fast the rest of the day.
How Intermittent Fasting affects Cardiovascular Health
Intermittent fasting (IF) has gained attention for its potential benefits on cardiovascular health, but its effects are still under investigation. Here’s how it can influence cardiovascular health:
- Improved Blood Pressure
- Cholesterol and Lipid Profile
- Reduced Inflammation
- Blood Sugar and Insulin Sensitivity
- Weight Loss and Fat Reduction
- Heart Rate Variability and Stress Management
- Autophagy and Heart Protection
- Potential Risks
Fasting appears to offer several cardiovascular health benefits, including improved blood pressure, cholesterol levels, and insulin sensitivity. However, it’s not a one-size-fits-all solution, and individual results may vary. Consulting with healthcare professionals can help determine if intermittent fasting is a suitable and beneficial approach to managing cardiovascular risk.
Research Studies on Intermittent Fasting and Cardiovascular Risk
Recent studies have examined how intermittent fasting might influence cardiovascular health. Here’s a summary of key findings:
Potential Benefits of Intermittent Fasting
Research suggests that intermittent fasting can lead to improvements in several cardiovascular risk factors, including reduced blood pressure, lower cholesterol levels, and decreased inflammation. For instance, a study published in Cell Metabolism found that intermittent fasting improved markers of heart disease in animal models, and similar results have been observed in human trials. It also helps in:
- Weight Loss and Fat Loss
- Improved Insulin Sensitivity
- Enhanced Heart Health
- Better Brain Health
- Longevity
Possible Risks and Considerations
While it shows promise, it’s not without risks. Some studies indicate that it might not be suitable for everyone, particularly those with existing heart conditions or those who are pregnant. In addition; excessive fasting could potentially lead to nutrient deficiencies if not managed properly like:
- Nutrient Deficiency
- Disordered Eating
- Impact on Physical Performance
- Not Suitable for Everyone
Tips for Safe and Effective Intermittent Fasting
- Start Slowly: Gradually introduce fasting periods to allow your body to adjust.
- Stay Hydrated: Drink plenty of water during fasting periods to stay hydrated.
- Eat Balanced Meals: Ensure your eating windows include a variety of nutrient-dense foods.
- Consult a Professional: Speak with a healthcare provider or nutritionist before starting, especially if you have underlying health conditions.
Expert Opinions and Recommendations
Experts suggest that it can be beneficial for cardiovascular health, provided it’s done correctly. Alternate-day fasting has shown potential in reducing cardiovascular risk factors, but it’s essential to approach it with caution and tailor it to individual health needs.
Best Practices for Combining Intermittent Fasting with Cardiovascular Health
- Monitor Your Progress: Regular check-ups to monitor heart health and adjust fasting practices accordingly.
- Focus on Nutrition: Combine fasting with a heart-healthy diet rich in fruits, vegetables, lean proteins, and whole grains.
- Stay Active: Complement fasting with regular physical activity to enhance overall cardiovascular health.
Additional Resources and Further Reading
For those interested in exploring intermittent fasting further, here are some valuable resources:
Online Tools and Communities: Join forums and online groups to connect with others practicing intermittent fasting and share experiences.
Conclusion
Alternate-day fasting holds potential benefits for cardiovascular health, including improvements in key risk factors. However, it’s essential to consider individual health conditions and approach fasting with proper guidance. By understanding the pros and cons and incorporating expert advice, you can make informed decisions about whether intermittent fasting is a suitable strategy for managing cardiovascular risk.
FAQs
Is intermittent fasting safe for the heart?
Intermittent fasting can be safe for heart health if done correctly. Consult with a healthcare provider to ensure it’s appropriate for your individual health needs.
Is intermittent fasting good for clogged arteries?
While intermittent fasting may help reduce risk factors associated with heart disease, it’s crucial to combine it with other heart-healthy practices and consult a healthcare professional.
Does fasting reduce cardiovascular disease?
Research indicates that intermittent fasting may reduce risk factors for cardiovascular disease, but more studies are needed to understand its long-term effects fully.
Does fasting improve cardio health?
Intermittent fasting may improve cardiovascular health by addressing risk factors such as high blood pressure and cholesterol levels. Always seek personalized advice from a healthcare provider.